Massage therapist SOAP notes example is essential for enhancing client care and session documentation.
However, therapists often face challenges ensuring comprehensive and transparent records for each session.
Massage therapists can improve communication and treatment outcomes by utilizing structured SOAP notes.
This blog post will guide readers through effectively creating and implementing these notes, featuring examples and practical tips.
SOAP notes are pivotal in tracking client progress and tailoring future sessions. They help therapists document subjective and objective information to assess and plan client care efficiently.
You can expect insights into crafting well-organized SOAP notes that accommodate client needs and therapist preferences.
This article incorporates examples and strategies to support massage therapists in refining their note-taking practices. This will enable better client interactions, facilitating ongoing evaluation and individualized care.
Understanding SOAP Notes
SOAP notes are an essential tool in healthcare for documenting patient interactions systematically.
They improve communication among healthcare providers by structuring important information. This organized approach ensures consistent and comprehensive patient care.
Basics of SOAP Format
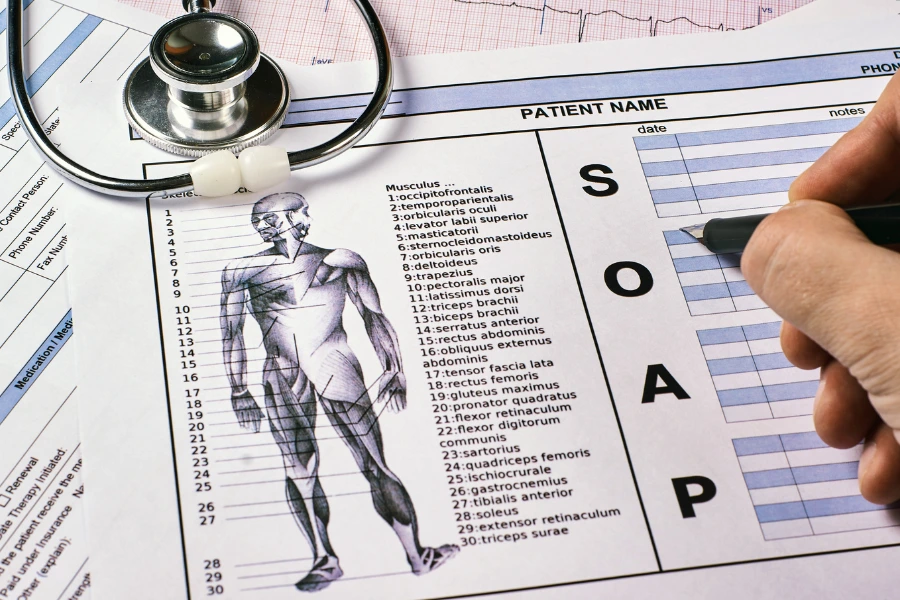
Health professionals, including massage therapists, use the SOAP format—which stands for Subjective, Objective, Assessment, and Plan—to record patient care.
- Subjective: This section records the client’s condition description, including any pain or discomfort. It may include patient quotes and a pain scale rating.
- Objective: Contains measurable data such as range of motion or muscle tension observed during the physical examination.
- Assessment: The therapist’s professional judgment about the client’s condition is based on subjective and objective findings.
- Plan: Outlines the treatment plan and any future sessions or referrals that may be necessary.
Importance in Client Care
SOAP notes play a critical role in effective client care. They ensure that massage therapy professionals and other healthcare providers communicate clearly about a client’s condition and progress.
Using SOAP notes aids in tracking a client’s progress and facilitates better treatment decisions.
It also enhances the treatment session by providing a transparent documentation process, helping identify changes in muscle tone or trigger points.
Additionally, they serve as a valuable resource for insurance providers, offering objective data that supports claims related to massage therapy practice.
The use of SOAP notes also helps maintain continuity of care during extended hours or when different therapists conduct sessions.
The Subjective Component
The Subjective Component of SOAP notes is crucial for understanding the client’s condition during massage therapy sessions.
It focuses on gathering detailed information from the client to ensure effective client care. This component is vital in forming a treatment plan with personalized attention.
Gathering Medical History
Healthcare professionals emphasize the importance of obtaining a thorough medical history. Massage therapists must learn about existing health conditions, medications, surgeries, or allergies that can influence treatment.
Clients often provide valuable information about previous injuries or chronic illnesses. Details about lifestyle factors, like long hours at a desk or strenuous physical activity, provide context.
A structured approach, such as digital soap notes or a soap note template, ensures that pertinent information is not overlooked.
Identifying the Chief Complaint
The chief complaint is the primary focus of the subjective section. It details why the client seeks massage therapy for pain relief or relaxation. The client’s description might include muscle tension, headaches, or back pain.
Massage therapy professionals often use questions to pinpoint the specific area of discomfort.
By documenting this effectively, the therapist can more accurately target treatment. Understanding the chief complaint helps develop an effective treatment plan that addresses the client’s concerns and goals.
Ensuring clarity in this section enhances the communication between client and therapist.
Assessing Pain Intensity and Client Communication
Clients often express their pain intensity using a pain scale of 1 to 10. This assessment is crucial to the subjective component, helping therapists gauge the severity and location of discomfort and adjust their treatment approach accordingly.
Recording feedback also helps audit the client’s progress and refine the treatment plan.
Utilizing mobile devices or massage therapy software can help maintain detailed notes. This practice supports better decision-making and continuity of care in future sessions.
The Objective Section
The Objective Section in SOAP notes is crucial for gathering factual information.
Observing and recording critical details about the client’s condition helps create a precise plan for patient care. This ensures effective communication among healthcare providers, improving treatment outcomes.
Objective Observations
In massage therapy, objective observations involve assessing the client’s physical state. This may include noting muscle tone, skin condition, or visible abnormalities.
Massage therapists often examine posture, gait, and movement patterns to identify areas of tension or imbalance in the body.
These observations form the basis for the client’s treatment plan and are critical in tailoring massage sessions.
Therapists look for specific triggers or knots that might need special attention during the assessment. Observations are not influenced by personal opinions, ensuring the information recorded is strictly factual.
Documenting Range of Motion
The objective section requires documenting the client’s range of motion (ROM). This involves measuring how well clients can move their joints and noting any restrictions or pain during movement.
Tests used to assess ROM provide valuable data that guide the massage therapy practice.
Therapists can identify areas requiring focus and adjust techniques accordingly, which is especially useful in cases like deep tissue massage.
Accurate documentation of ROM is vital for practical SOAP notes. Healthcare professionals use this information to monitor progress across future sessions, ensuring that therapy is beneficial and targeted.
Recording Vital Signs
Recording vital signs using SOAP notes is standard practice for many healthcare professionals. While not always required in massage therapy, these records provide essential information about the client’s health status.
Vital signs can include heart rate, blood pressure, and temperature, which might be relevant for clients with specific health conditions.
This part of the objective section adds depth to the overall documentation process. When combined with other observations, vital signs contribute to a comprehensive understanding of the client’s condition, enhancing the quality of care.
Professionals may rely on massage therapy software to streamline the data collection and keep accurate records.
Assessment Strategies
Massage therapists must evaluate muscle tension and trigger points for effective client care. This process is crucial for determining treatment effectiveness and tailoring a personalized treatment plan to address the client’s condition.
Evaluating Muscle Tension and Trigger Points
Identifying muscle tension and trigger points is a crucial part of the assessment section in massage therapy SOAP notes.
Health care providers focus on these areas to determine the regions where clients may experience discomfort or restricted movement.
By documenting the client’s response to touch and pressure, practitioners can gather objective data on affected muscles.
Massage therapy professionals often use palpation and range of motion tests to observe muscle tone and flexibility.
This detailed assessment highlights essential information about trigger points and helps tailor future sessions for better results.
Regularly updating massage SOAP notes ensures crucial information is communicated effectively among healthcare professionals and is valuable for insurance companies processing client progress.
Determining Treatment Effectiveness
Evaluating treatment effectiveness involves reviewing the subjective and objective components of soap notes.
Clients report their experience, pain relief, and progress since the last visit, contributing subjective input necessary for a comprehensive assessment.
Healthcare providers then compare this feedback with objective information gathered during the physical examination.
By analyzing this data, massage therapists can adjust the treatment plan to meet client needs effectively.
Patient progress is monitored over multiple massage sessions, ensuring beneficial treatment.
Massage therapy software can enhance this data collection, enabling professionals to track objective section entries and client reports efficiently. It is a valuable resource for improving patient care and ensuring positive responses.
Using a structured approach in documenting treatment effectiveness helps massage therapy practitioners deliver targeted, client-specific solutions.
Developing the Treatment Plan
A well-crafted treatment plan in massage therapy is essential for guiding sessions and achieving client goals. This includes using clinical techniques and setting clear expectations.
Incorporating Clinical Techniques
Massage therapists use different techniques in their treatment plans to address the client’s specific needs.
When writing the treatment plan in massage therapy SOAP notes, practitioners focus on techniques suited for the client’s condition, like deep tissue massage for muscle tension.
Including effective techniques helps healthcare professionals provide better patient care. Techniques should be based on the client’s description and assessment findings.
It’s important to note any specific area of concern so that future sessions can be tailored accordingly. Incorporating this information ensures a structured approach, promoting effective communication and patient progress.
Setting Goals and Expectations
Setting clear goals and expectations in the treatment plan is vital for the therapist and the client.
Goals like improving range of motion or reducing pain levels should be measurable, often recorded in the objective section of SOAP notes.
To ensure a shared vision, clients and therapists discuss these goals during massage therapy sessions.
A SOAP note template can help maintain a consistent format for tracking progress.
This allows healthcare providers to adjust techniques based on the client’s response. Regularly revisiting these goals ensures the treatment plan remains relevant and practical.
Maintaining detailed notes also helps provide valuable documentation for insurance companies and other third parties that may require proof of patient care.
Execution and Documentation
Massage therapists utilize SOAP notes to enhance client care and streamline documentation.
Understanding how to apply massage techniques effectively and document them in SOAP notes is crucial for successful treatments and communication among healthcare providers.
Applying Massage Techniques
The therapist begins each massage session by evaluating the client’s condition. This may include listening to the client’s pain or discomfort and performing a physical examination.
The therapist focuses on specific areas that require attention, like muscle tension or trigger points.
Techniques such as deep tissue massage might address muscle tone and improve the client’s range of motion.
The treatment plan is tailored to the client’s needs, ensuring each session contributes positively to their well-being.
By keeping a structured approach, therapists can efficiently target problem areas, improving client satisfaction and effective treatment outcomes.
This approach addresses the immediate concerns and sets a foundation for future sessions.
SOAP Notes for Each Session
Massage therapy SOAP notes are essential for documenting each session. The notes use a standardized SOAP format for Subjective, Objective, Assessment, and Plan.
In the subjective section, the client reports their chief complaint and any pertinent information, providing valuable insights into their condition.
The objective section records measurable data, such as muscle tension or pain scale.
The therapist evaluates the client’s progress in the assessment section and observes any changes since the last visit. The plan section outlines future sessions and treatment strategies to maintain or enhance the client’s progress.
Utilizing digital SOAP notes can help massage therapy professionals organize important information and communicate effectively with healthcare providers. This efficiency is crucial when submitting documentation to insurance companies.
For detailed resources, therapists may refer to platforms like MBLExGuide and GlossGenius.
massage therapist soap notes example: Technological Integration
Technology has greatly enhanced how massage therapy professionals document and manage SOAP notes.
With the rise of digital tools, capturing and maintaining detailed notes has become more efficient, benefiting both therapists and clients.
Using SOAP Notes Software
Massage therapists can improve their documentation with SOAP notes software. This technology streamlines the documentation process by offering structured templates covering subjective, objective, assessment, and plan sections.
These templates ensure consistent and accurate record-keeping.
Software solutions often include features like automated reminders for future sessions, which help therapists maintain effective communication and continuity of care.
Mobile devices allow therapists to input data quickly during or after treatment sessions, capturing essential information such as the client’s condition and objective data.
Moreover, digital SOAP notes facilitate secure storage and easy sharing with other healthcare providers when necessary.
This integration enhances patient care and allows therapists to focus more on the client during sessions rather than spending long hours on paperwork afterward.
Technology helps ensure the documentation is error-free and accessible, improving overall client sessions and client progress tracking.
Collaboration and Referrals
Practical SOAP notes ensure seamless collaboration and referral processes between massage therapists and other healthcare providers.
These notes help maintain effective communication, enhance patient care, and facilitate smooth transitions in treatment plans.
Working with Healthcare Providers
Massage therapists often work alongside healthcare professionals like doctors, chiropractors, and physical therapists. Sharing detailed SOAP notes ensures all parties are informed about the client’s condition and progress.
Objective information from massage sessions, such as changes in muscle tone or range of motion, can provide valuable insights. When therapists record these details, they help other health care providers make informed decisions.
SOAP notes also support communication about the client’s response to treatment, which is crucial for adjusting care plans.
Referral Process and Continuity of Care
Effective referrals require essential information about the client’s progress and treatment sessions.
Massage therapy SOAP notes often include the subjective component, where clients describe their symptoms or pain scale, and the objective section, where therapists document observations and assessments.
During referrals, therapists must share pertinent information about the outcomes from previous treatments and any adverse reactions the client may have experienced.
These details help the next provider understand the client’s history and ensure continuity of care.
Insurers and other third parties may also rely on these notes to validate the necessity and effectiveness of ongoing care.
By following best practices in documenting SOAP notes, therapists can enhance their collaboration with other health professionals and ensure that the client’s care is coordinated and effective.
Aftercare and Client Education
After a massage therapy session, clients need proper guidance to continue their care at home. Providing self-care recommendations and ergonomic advice can help maintain the treatment’s benefits and support long-term wellness.
Self-Care Recommendations
Massage therapists often advise clients on how to continue their care outside the clinic.
Suggestions can include stretching exercises to improve flexibility and range of motion. Recommending specific exercises can help maintain muscle tone and further relieve tension.
Clients may also be advised to apply heat or ice to the treated area, depending on their specific needs. This can help reduce muscle tension or inflammation.
Therapists record these recommendations in the plan section of their SOAP notes, ensuring that this critical information is documented for future sessions.
This detailed approach benefits both the client and the therapist by improving the effectiveness of ongoing treatment plans.
Guidance on Ergonomics
It is essential to educate clients on proper ergonomics, especially those who experience pain after work due to long hours at a desk.
Healthcare professionals can guide workspace setup to minimize strain on the body.
Adjusting chair height, monitor level and keyboard placement can significantly impact a client’s condition.
Healthcare providers may also recommend periodic breaks and simple stretching routines during work to alleviate stress and muscle fatigue.
Including these recommendations in the objective section of the massage therapy SOAP notes ensures they are part of the structured approach to patient care and reflect best practices in massage therapy sessions.
Last Words
Massage therapists and SOAP note examples are vital in maintaining clear communication and effective treatment plans.
By structuring notes using the Subjective, Objective, Assessment, and Plan (SOAP) format, therapists ensure that each client’s session is well-documented and individualized.
Subjective: This includes the client’s reported symptoms or concerns. For instance, a client might mention persistent lower back pain.
Objective: This section comprises observable findings.
It could involve noting any tight muscle areas or visible discomfort during massage.
Assessment: The therapist evaluates and interprets the findings. For example, they may determine that new discomfort requires additional shoulder therapy.
Plan: Here, the future treatment strategy is outlined. The therapist may suggest techniques or session frequency to address identified issues.
Using these SOAP notes helps streamline the documentation process, making it efficient and easy for any therapist to follow.
Moreover, SOAP Note AI offers tools to automate part of this process.
By consistently using SOAP notes, therapists can improve patient outcomes and enhance their practice’s professionalism.
Additionally, exploring other health documentation practices on knowyourhealing.com can provide further insights into integrating these methods effectively.